Home · Book Reports · 2024 · Melatonin - Your Body's Natural Wonder Drug
- Author :: Russel J. Reiter
- Publication Year :: 1995
- Source :: Melatonin_your_bodys_natural_wonder_drug_(1995).pdf
designates my notes. / designates important. / designates very important.
Page numbers from the book, not pdf.
Thoughts
I have been taking 5mg of melatonin nightly, about 1.5 hours before bed, for the last 4 months. It helps me fall asleep only in a minor way, but it helps me sleep a full 8 hours. My sleep schedule fluctuates (with my mood, bi-polar) from 6 hours during a high energy (mania) period, to 10 hours during a low energy (depressed) period. This would wreak havoc on my sleep/wake times. With melatonin I was able to sleep 8 hours when I would only expect 6, and in my depressed period occurring now I am averaging a little over 9 hours per night.
I can’t speak to any of the other benefits, but the leveling out of my sleep is enough benefit for me to continue using it nightly.
The anti-oxidant effects seem like an open and shut case and nothing remotely controversial. I also take beet root powder (juice) that contains Nitric Oxide. This is highly reactive and anti-oxidants in general should improve its function.
If even a fraction of the other benefits are true, it is worth the 1-2 dollars a month that this supplement costs given there are essentially no negative side effects.
Exceptional Quotes
This study and similar ones showed that melatonin has many of the opposite effects of adrenaline. Adrenaline increases the heart rate, tenses the muscles, raises the blood pressure, and compels one to take action. By contrast, melatonin lowers the heart rate, relaxes the muscles, and lulls one to sleep. If adrenaline is the “fight-or-flight” hormone, then melatonin is the “rest-and-recuperate” hormone.
melatonin is not just an antioxidant—it appears to be the most efficient and versatile antioxidant known. It is twice as effective as vitamin E, five times as efficient as glutathione, and five hundred times more effective than the synthetic antioxidant DMSO.
Melatonin is both fat and water solublea rare occurrence in nature—making it the only known antioxidant that can protect all parts of the cell.9 Furthermore, because melatonin can navigate all the barriers in the body with ease, including the blood-brain barrier and the placental barrier (which protects the unborn child), the antioxidant-hormone can protect every cell in the body.
Another reason that melatonin is such a superlative sleep aid is that it does not lose its effectiveness over time. Benzodiazepines can become less effective after only two or three nights of use. By contrast, melatonin may become a more effective sleep aid with chronic use. In an Israeli study, researchers gave 2-milligram doses of melatonin to elderly volunteers for two months. At the end of the treatment period, the volunteers fell asleep even more quickly than they did after one week of treatment. 19
The preliminary data from this study shows that melatonin is just as effective as temazepam in reducing the amount of time it takes the subjects to fall asleep. It also extends sleep the same amount of time. But unlike temazepam, melatonin does not delay REM sleep, and therefore it results in a more normal sleep architecture.29
A paper published by an Israeli group in 1995 showed that giving melatonin on a nightly basis to aging rats prevented the age-related decline in testosterone production. In fact, the melatonin-treated rats had almost three times as much testosterone as those not given the hormone. 20
no pharmaceutical company has shown a great interest in melatonin research because the molecule cannot be patented.
Table of Contents
- 00: Introduction
- 01: Meet Melatonin, the Life-Giving Molecule
- 02: The Three-Billion-Year Old Molecule
- 03: The Best Antioxidant
- 04: Boosting the Immune System
- 05: New Hope For AIDS Patients
- 06: Taming the Savage Cell
- 07: Protecting Your Heart
- 08: Unlocking the Sleep Gate
- 09: Back in Sync
- 10: A Master Sex Hormone
- 11: Melatonin and Your Mind
- 12: The Great Anti-Aging Experiment
- 13: Let There Be Light And Dark
- 14: The Elusive Enemy- Electromagnetic Fields
- 15: Drugs That Deplete Melatonin
- 16: Creating a Melatonin Friendly Lifestyle
- 17: Taking Melatonin Supplements
- 18: When God Holds the Patent
Part 1 - Your Body’s Natural Wonder Drug
Part 2 - Attaining Healthy Levels of Melatonin
Part 3 - The Future of Melatonin Research
Part 1 - Your Body’s Natural Wonder Drug
· Chapter 1 - Meet Melatonin, the Life-Giving Molecule
page 3:
-
In the exact center of your brain resides a tiny organ called the pineal (pronounced “pie-NEEL”) gland, which is about the size and shape of a kernel of corn.
-
The pineal was the first gland in your body to be formed, clearly distinguishable a mere three weeks after conception.
page 5:
-
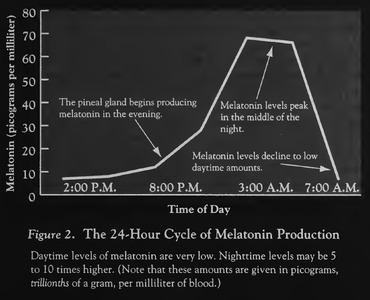
At around two or three in the morning, when your melatonin levels peak, there is a significant increase in the number of immune cells circulating in your bloodstream, enhancing your body’s defenses against cancer, viruses, and bacteria.
-
Melatonin also plays a vital role in boosting your immune system when you are under stress, whether that stress comes from viral infection, emotional stress, drugs that suppress the immune system, or the aging process.
page 6:
- In 1993 my colleagues and I at UTHSC discovered that melatonin is the most potent and versatile of all the known antioxidants.
page 7:
-
Melatonin lowers cholesterol and blood pressure, researchers have found, and reduces the risk of irregular heartbeat. In one pilot study, melatonin normalized the blood pressure of people with hypertension within a week, with no negative side effects.
-
Compelling new evidence suggests that melatonin plays a primary role in the body’s defense against cancer. In a number of studies, when animals were protected with melatonin before being injected with a potent carcinogen, cancer failed to develop.
-
Melatonin may also slow the growth of cancer once it is established. Test-tube studies have demonstrated that melatonin inhibits the growth of a number of human cancer cells, including breast cancer, lung cancer, cervical cancer, melanoma, and most recently, prostate cancer.
page 9:
-
Taking melatonin may extend your healthy, productive life span. As you age, your body produces less and less melatonin, depriving you of this sleep- enhancing, free-radical-scavenging, heart-calming, immune-stimulating, cancer-fighting hormonein short, depriving you of one of your best defenses against aging. Replenishing your supply of this vital hormone may allow you to live longer and delay the onset of crippling diseases such as arthritis, diabetes, heart disease, cancer, Alzheimer’s, and Parkinson’s. This possibility is more than wishful thinking. In laboratory studies, giving melatonin to aging animals has extended their life span by as much as 20 percent.
-
the body produces very little melatonin in the daytime. If you take a melatonin tablet at the wrong time of day, you work at cross-purposes to your natural biological rhythms. Even more troubling, children produce ample amounts of melatonin on their own. Except in rare instances—and then only under a doctor’s super- vision—there is no reason to give children melatonin.
page 11:
- I sense a major shift in popular thinking about health care. Many people no longer believe that their family physician has the answers to all their health questions. In their passion to get well or stay well, they are pursuing medical information on their own, through magazines, books, excursions on the Internet and by braving the scientific literature itself.
· Chapter 2 - The Three-Billion-Year Old Molecule
page 12:
- melatonin is a very old molecule. It has been found in every animal and plant studied to date, from human beings to the most primitive one-celled algae that evolved more than three billion years ago.
page 15:
- Try as they might, the researchers could not determine the LD50 for melatonin, even though they injected mice with as much as 800 milligrams of it per kilogram of body weight, which for adult humans would be equivalent to injecting a half-cup of pure melatonin.
page 16:
-
Through our work with hibernating hamsters, we learned that melatonin triggers the seasonal breeding of animals.
-
Melatonin, however, presented an even greater challenge because it is produced in picograms — trillionths of a gram!—the smallest amount of any known hormone.
page 17:
-
he injected them with as much as 75 milligrams of melatonin. Within minutes of receiving the injections, the patients began producing slower brain waves—a sign of tranquillity. Soon most of them were sound asleep. When Anton-Tay awakened them about forty-five minutes later, they reported having unusually vivid dreams and experiencing a sense of “well-being and moderate elation.“8
-
This study and similar ones showed that melatonin has many of the opposite effects of adrenaline. Adrenaline increases the heart rate, tenses the muscles, raises the blood pressure, and compels one to take action. By contrast, melatonin lowers the heart rate, relaxes the muscles, and lulls one to sleep. If adrenaline is the “fight-or-flight” hormone, then melatonin is the “rest-and-recuperate” hormone.
page 18:
-
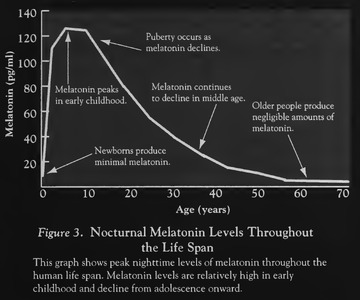
Production of it varies considerably over the life span. Newborns produce very little melatonin, we found, until around three months of age. Three months happens to be the stage of development when they begin to sleep longer stretches at night and to be more alert during the daytime. We began to suspect that melatonin might be the underlying reason for this regularity. Once babies produce a strong nocturnal surge of melatonin, they have a hormonal pacemaker that helps them tell night from day.
-
Babies produce increasing amounts of melatonin, we learned, until they are about one year old. Then their nocturnal melatonin levels remain steady until just before puberty, when they decline markedly, a trend that continues for the next five years or so.9 This steep decline got us to wondering if a falling concentration of melatonin helps trigger the onset of puberty. 10 In animals, high levels of melatonin are known to inhibit reproduction. Do human melatonin levels have to go down before we become sexually mature? Some researchers argued they do, while others shot the notion down.
page 19:
- As you can see in the graph in Figure 3, the body’s production of melatonin declines inexorably with age. A seventy- or eighty-year-old may have the hormone in amounts so small as to be undetectable. A nuniber of hormones decline with age, including testosterone, estrogen, growth hormone, and DHEA (dehydroepiandrosterone), which is a precursor of the sex hormones. The gradual loss of these hormones was once seen as a consequence of aging. Now researchers are beginning to suspect their loss may contribute to the aging process, and that replacing them may extend our youth. Preliminary studies suggest that they are right. But of all the hormones, melatonin appears to have the greatest anti-aging potential, a subject to be explored in Chapter 12.
page 20:
- One of the reasons that melatonin has so many rejuvenating powers is that it protects and enhances the immune system, especially in aging organisms.
page 22:
- melatonin is not just an antioxidant—it appears to be the most efficient and versatile antioxidant known. It is twice as effective as vitamin E, five times as efficient as glutathione, and five hundred times more effective than the synthetic antioxidant DMSO.
· Chapter 3 - The Best Antioxidant
page 24:
- Right now, as you read this page, melatonin in your blood is preventing the oxidation of LDL cholesterol, the “bad” cholesterol that can clog your arteries. Melatonin in your brain is safeguarding your irreplaceable neurons from free-radical attack. Melatonin in the fluid within your eyes is helping to prevent free radicals from forming cataracts. Melatonin in the lining of your gut is reducing your risk of ulcers.
page 25:
- Their research suggests that free radicals cause or exacerbate a rogue’s gallery of diseases including cancer, AIDS, asthma, adult respiratory distress syndrome, cataracts, emphysema, fetal alcohol syndrome, heart disease, macular degeneration, stroke, ulcers, Alzheimer’s, Parkinson’s, and rheumatoid arthritis. Furthermore, researchers have produced convincing evidence that free radicals play a major role in the aging process itself.1
page 27:
- There are two major sources of antioxidants those that you get from food or food supplements (vitamins E, C, and beta-carotene, for example), and those that are produced within your own body. The antioxidants you produce inside your body are less well known but just as vital. They include molecules such as glutathione and uric acid, which scavenge free radicals directly, and antioxidative enzymes such as glutathione peroxidase, catalase and superoxide dismutase (SOD), which break them down into nontoxic products. Melatonin is a new star on this scene.
page 28:
-
At UTHSC, my postdoctoral fellows and I found that melatonin may help prevent cancer by serving as DNA’s personal bodyguard. We made this discovery by injecting rats with safrole, a toxic substance known to cause cancer by unleashing large amounts of free radicals. We injected half of these rats with melatonin as well. Twenty-four hours later, we examined their liver cells for DNA damage. The animals that had been given safrole alone had sustained significant damage to their DNA; if the experiment had continued, many of them would have developed liver cancer. Careful measurements revealed that the DNA of the melatonin-treated rats had sustained only 1 percent as much damage. (See Figure 5.)
-
Another experiment that was of special interest to me is one in which we showed that melatonin protects human white blood cells from radiation.
page 29:
- To see if melatonin could prevent this type of free-radical damage, my colleagues and 1 exposed human white blood cells to radiation. At the conclusion of the experiment, we found that melatonin protected the cells better than any other known antioxidant. Remarkably, it was five hundred times more effective than the synthetic antioxidant DMSO, which is regarded as an excellent radioprotector.6
page 30:
-
In 1993 a postdoctoral student named Mitshube Abe, M.D., was working in my lab. Abe’s field was ophthalmology, and he wanted to see if melatonin could protect the eyes from free radicals. The lens of the eye is approximately 98 percent protein. When the protein becomes damaged by free radicals, it coagulates, making it opaque. The result is cataracts. (This is very similar to what happens when you fry the white of an egg.) The older you are, the longer your eyes have been exposed to UV light from the sun, and the more likely you are to have cataracts.
-
Somehow your body “knows” that your eyes are vulnerable to free- radical damage, and it provides them with an extra helping of antioxi- dants—a built-in pair of sunglasses. Melatonin is especially abundant in the eye. As you age, however, you produce less and less melatonin, which may make you more and more vulnerable to cataracts.
-
Abe worked with a group of young rats that had been depleted of their supply of glutathione, one of the important antioxidants produced in the body. (Like melatonin, glutathione has been found in virtually all organisms.) Young rats that are made glutathione-deficient form cataracts in as little as two weeks. We gave half of these rats melatonin to see if it could prevent them from forming. Sixteen days later, we examined the animals and found that the rats that were not given melatonin had cataracts in both eyes; in the melatonin-treated group, only one rat had a cataract, and that was just in one eye.
-
This is another study with obvious clinical applications, as Abe suggests in a recent paper:
- Considering that senile cataracts in the human are considered to be the result of oxidative stress … it is possible that supple- menting elderly individuals with melatonin, which is normally lost during aging, may delay and/or prevent cataract development normally associated with aging.
page 31:
- Evidence shows that melatonin crosses the blood-brain barrier with ease. We demonstrated this fact in our most recent antioxidant experiment, in which we found that melatonin protects the brain from free radicals generated by stroke.
page 32:
-
melatonin prevents free-radical damage caused by the toxic pesticide paraquat; protects the stomach from the corrosive effects of alcohol; and prevents damage caused by the bacterial toxin (LPS) that causes toxic shock and sepsis. Whenever we have pitted melatonin against a free-radical foe, melatonin has been the winner by a knockout.
-
Melatonin is both fat and water solublea rare occurrence in nature—making it the only known antioxidant that can protect all parts of the cell.9 Furthermore, because melatonin can navigate all the barriers in the body with ease, including the blood-brain barrier and the placental barrier (which protects the unborn child), the antioxidant-hormone can protect every cell in the body.
page 33:
- Melatonin appears to have none of these drawbacks. It has little or no toxicity, not even in megadoses;
· Chapter 4 - Boosting the Immune System
page 36:
-
Studies have shown that you can influence your health by practicing meditation or visual imagery, having a deep religious faith, belonging to a supportive network of family and friends, or learning to think more positively.1 Even fleeting emotions can boost your immunity, a fact that can be verified under a microscope. In a recent study, groups of volunteers were shown either of two documentaries: one an uplifting film about Mother Teresa, and the other a comparatively bland nature film. Blood samples were drawn from the volunteers before and after each viewing. The volunteers who watched the inspiring story about Mother Teresa had a significantly greater increase in white blood cells than those who watched the nature film.
-
Correspondingly, negative thoughts and feelings have been shown to have a negative impact on your health. Statistically, people who have been recently widowed are more likely to die in the year following the death of the spouse. More recently, people infected with HIV who show signs of depression have been found to have a poorer prognosis than those who do not.2 The fact that depressed people are more vulnerable to disease may be due, in part, to the fact they have a deficiency of “natural killer cells,” a class of immune cell that protects the body against cancer and viruses.3
-
How do moods, those ephemeral blends of thoughts and feelings, influence immune cells? Our understanding is incomplete, but researchers have discovered that certain immune cells have receptors (or docking stations) for neurotransmitters, the substances that transmit impulses between nerve cells and play a determining role in one’s state of mind. (Serotonin and dopamine are examples of neurotransmitters.) When you are depressed, a deficiency of neurotransmitters interferes with the flow of messages between your brain cells. As a result, you feel sluggish and unmotivated and have less ability to experience joy. This same deficiency of neurotransmitters is detected by your immune cells, and in ways not fully understood, it results in a depressed immune system as well as a depressed mood.
page 37:
-
Testosterone, which is considered a male sex hormone because it is more abundant in men than in women, actually inhibits the immune system. In a number of studies, male animals that have been castrated (which eliminates the production of testosterone) had a lower incidence of disease than did intact animals. They also lived longer.4
-
Estrogen, a hormone that is more abundant in women than in men, plays a complex role in the immune system. It reduces a woman’s risk of acquiring some diseases but increases her risk of acquiring others. Women as a group are more resistant than men to infectious diseases, but they are more likely to be afflicted with autoimmune diseases. Women have twice the rate of multiple sclerosis, three times the rate of rheumatoid arthritis, and nine times the rate of systemic lupus, a disease that attacks the connective tissues of the body.
-
Stress hormones are without gender bias—they occur in both men and women and dampen the immune response of both. You may have noticed that when you are under prolonged stress, you are more likely to get sick and may take longer to recover. Both physical and mental stress increase your production of a hormone called Cortisol. Your immune cells have receptors for Cortisol, and when Cortisol links with those cells, it slows down their rate of division, leaving your immune system shorthanded.5
-
Intuitively, it would seem that a weakened immune system might make it more difficult to survive a stressful episode. But the net effect of the stress hormones is to enhance your survival. When you are under acute stress, the stress hormones divert your energy away from nonessential functions such as reproduction and the healing process and toward your muscles; when you are running away from a predator, you don’t want your body to be preoccupied with fighting off a minor cold or distracted by thoughts of mating.
page 38:
-
The rats that were experimented on from 1965-85 didn’t show signs of melatonin’s benefits because they were basically young, healthy, and stress free.
-
All told, the rats experienced far less stress than they would have in the wild. They had no need to hide from enemies, no reason to forage for food, no exposure to inclement weather, and less contact with dust, bacteria, vermin, and viruses than those of us who were studying them. The only significant stress in their lives was confinement and boredom.6
page 42:
-
You produce two main types of T cells: T-killer cells, which are a part of the attack team, and T-helper cells, which direct the whole operation. T-helper cells coordinate other cells in the immune system by producing a family of intercellular signaling substances called cytokines. Each cytokine regulates a different set of cells, suppressing the growth of some and stimulating the growth of others. (Cytokines include the interleukins, interferons, colony-stimulating factors, and tumor necrosis factors.) Without T-helper cells coordinating the immune system, the battle would be lost. It would be as if you were trying to fight a war when your entire communication network has broken down.
-
Maestroni’s and Conti’s breakthrough discovery is that there are melatonin receptors on T-helper cells. When a cell has a receptor for a given hormone, it implies that the hormone plays a significant role in regulating that cell.
page 43:
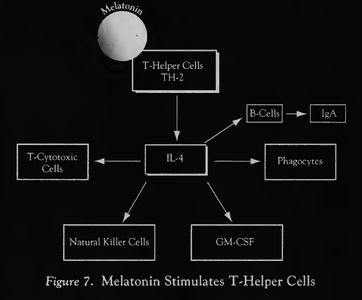
- As you can see by Figure 7, one type of cell that is stimulated by melatonin is the natural killer cell, or NK cell. NK cells specialize in attacking two of your body’s stealthiest invaders—cancer cells and virus-infected cells. These particular enemies are very difficult for your surveillance system to detect because they camouflage themselves as healthy cells. Viruses hide deep within a cell, commandeering its internal machinery to make clones of themselves, leaving few traces on the outside of the cell to betray their presence. Cancer cells are just as devious in that they retain virtually all the external markings of the healthy cells from which they sprang. Identifying a virus-infected cell or a malignant cell is like trying to distinguish between friend and foe on a battlefield when both sides are wearing the same uniform. Fortunately, your NK cells have mastered the art. Taking small amounts of melatonin can cause a dramatic increase in your production of NK cells. In a study published in 1994, six healthy young men took 2 milligrams of melatonin each night for a period of two months. Their NK cells were measured before and after the study. At the end of the treatment period, the men were producing an average of 240 percent more NK cells, more than doubling their arsenal against cancers and viruses. 16
page 45:
-
Maestroni and Conti announced in 1995 that melatonin promotes the growth of bone marrow cells.18 There are many instances when the ability to stimulate bone marrow cells would prove invaluable. One obvious instance is during chemotherapy. Most of the drugs used to destroy cancer cells are toxic to the bone marrow, resulting in the loss of a great number of white blood cells. Other people who could benefit from a substance that stimulates bone marrow cells are the millions of people with depressed immune systems due to aging, stress, or chronic disease.
-
To understand how melatonin stimulates bone marrow cells is to gain insight into the complexity and interdependence of the immune system. Essentially, melatonin functions as the first runner in a well-trained relay team. To set the race in motion, melatonin links with its receptor on the T-helper cell. The T-helper cell is the next team player, producing more of the IL-4-like factor. This factor then takes the baton and stimulates the production of a substance called granulocyte-macrophage colony-stimulating factor, which (mercifully) is referred to as GM-CSF. GM-CSF, the last runner in the team, sends a stimulatory message to stem cells located in he bone marrow. 19 The net effect of this cooperative venture is that you have a new bounty of white blood cells to help protect you from disease.
· Chapter 5 - New Hope For AIDS Patients
page 47:
-
Data published in 1995 reveals a strikingly different view of the disease. Researchers now believe that the virus replicates at a furious pace from the moment of infection, churning out as many as 2 billion new viral particles each day.1 The reason that the patient remains symptom free for some time is that the immune system is creating new cells at an equally impressive rate. This silent invisible battle rages for years. As long as the two forces are of comparable strength, the patient has few symptoms, thus giving the false impression that the virus is dormant.
-
Inside each of us there are two gay wolves.
· Chapter 6 - Taming the Savage Cell
page 62:
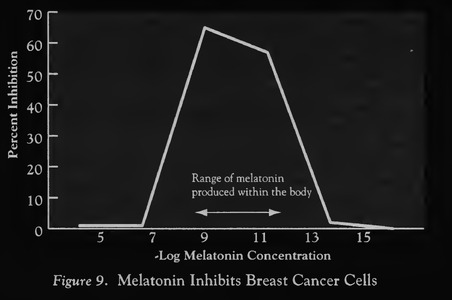
- Assisted by post-doctoral student Steven Hill, Blask divided the breast cancer cells into two groups. Their plan was to add melatonin to one of the batches of cells. If melatonin had an inhibitory effect, those cells should divide at a slower rate than the untreated batch. Not knowing how much melatonin to add, Blask and Hill added a relatively large amount. In Blask’s own words, “like any good chemists we dumped in a bunch of melatonin.” They wanted to make sure that any potential effect would be perceptible. But even though the cells were exposed to a hundred times more melatonin than is present in the human bloodstream, they continued to thrive.
page 63:
-
The researchers repeated the experiment a number of times and came up with the same results: There was no difference in the rate of growth between the cells that were growing with and without melatonin. Blask and Hill were about to conclude that melatonin had no effect on the cells when it dawned on Blask that they might be using too much melatonin. Maybe less is more," he suggested to Hill. “The body produces so little of it, maybe it works best in small quantities.” They went back to the lab and repeated the experiment, using much smaller amounts of the hormone. To their surprise, a mere smattering of melatonin blocked the growth of the breast cancer cells by 75 percent. This finding was unexpected since virtually all anticancer compounds are most effective in high concentrations. Melatonin apparently works the other way around.
-
Intrigued, Blask and Hill went on to see if they could determine the most effective concentration of melatonin. This phase of the study produced an even more remarkable finding: Melatonin had the greatest effect in a very particular range—a range that happens to be the amount of melatonin present in the human body. Concentrations above and below that amount had no effect on the cells."4 “We were stunned,” Blask says. “We had a phenomenon we couldn’t explain. It was easy to understand why very small concentrations of melatonin had no effect. But why were high amounts ineffective? All that we knew was that, for some reason, a woman’s body produces precisely the amount of melatonin required to slow the growth of these breast cancer cells. The body knew something that we didn’t.”
page 64:
- Cos obtained clones of the same breast cancer cells used by Blask and Hill. After dividing them into a number of different groups, he incubated each group in a different manner. Some he incubated continuously in the amount of melatonin the body produces at night, others in daytime concentrations. Still others were incubated in alternating concentrations — high for twelve hours and then low for twelve hours—replicating the body’s circadian cycle. As Cos had surmised, the cancer cells that showed the least growth were the ones incubated in the alternating concentrations.5 Once again, mimicking the body’s own strategy had produced the best results.
page 68:
- New, as yet unpublished data shows that melatonin inhibits the growth of prostate cancer cells. When David Blask and another group of researchers incubated human prostate cancer cells in melatonin, they got a 50 percent inhibition.17
page 69:
- Another similarity between breast cancer and prostate cancer is that some studies have shown that people who have these diseases have unusually low levels of melatonin. Whether the low levels of melatonin contribute to the disease or are a result of it is not yet known.
page 71:
- In 1990 he began experimenting with just such a therapy—combining melatonin with interleukin-2. A natural component of the immune system, IL-2 is a signaling compound that stimulates the growth of the body’s immune cells. For this reason, it had been under investigation as a treatment for cancer for a number of years. It was effective in treating a few kinds of cancer, primarily melanoma and renal cancer, but in the doses required to get a response, it was toxic. It was not unusual for patients to die from the treatment itself. Lissoni hoped that combining melatonin with IL-2 would allow for a much lower dose of IL-2, reducing the toxicity of the treatment without compromising its effectiveness. 20
page 72:
-
As he hoped, melatonin plus IL-Z proved a far superior treatment to IL-2 alone. Figure 12 compares the average immune response of ninety consecutive cancer patients who were given IL-2 plus melatonin with forty patients who were given IL-2 alone. 21 As you can see, adding melatonin to the treatment had a much greater stimulatory effect on the immune system.
-
The new combination therapy reduced the toxicity of IL-2 to such an extent that some of the patients were able to administer the treatment themselves at home. Each night, they would give themselves a low-dose injection of IL-2 22 and swallow a 40-milligram tablet of melatonin. This simple treatment allowed them to remain in the comfort of their own homes and saved them a great deal of money.
-
But how good was this home therapy? Compared with melatonin alone, melatonin plus IL-2 proved to be much more effective. More patients responded to the treatment, they experienced a greater reduction in tumor size, and for the first time, a few patients had complete regression of their tumors.

page 73:
-
How did this therapy compare with IL-2 alone? To find out, Lissoni and his colleagues enrolled eighty patients in a randomized study. 23 IL-2 plus melatonin proved the superior treatment in every regard. For exam- ple, three patients in the IL-2 plus melatonin group underwent complete regression of their tumors, while none did in the IL-2 group. Twenty-seven percent of those given IL-2 plus melatonin had a significant reduction in tumor growth, compared with only 2 percent of the IL-2 group. In terms of survival, IL-2 plus melatonin was also clearly superior. One year after the start of the trial, 46 percent of the patients in the IL-2 plus melatonin group were still alive, compared with only 15 percent in the IL-2 group. 24
-
This particular study involved sixty patients with advanced lung cancer—a disease with a poor prognosis. Half of the patients were treated with a widely used chemotherapy regimen, cisplatin and etoposide.‘25 The other half were treated with IL-2 plus melatonin. In assessing any new therapy, two main factors are considered: the quality of life of the patients after treatment, and their survival time. IL-2 plus melatonin proved superior for both factors. At the end of one year, 45 percent of those receiving the immunotherapy were still alive, compared with only 19 percent of those receiving chemotherapy. The group receiving the immunotherapy also had fewer side effects. For example, none of the patients treated with IL-2 plus melatonin experienced any vomiting, toxicity to the cardiovascular system, or blood cell abnormalities—reactions that were commonplace in the chemotherapy group. 26
page 75:
-
He and Gonzalez enrolled forty-two patients with advanced melanoma for the study. On average, the patients had a life expectancy of only six months. “At this point in their treatment,” says Gonzalez, “you are grasping for straws.” In fact, three patients died within two weeks of joining the study. Each day, the patients were given melatonin in tablet form, the doses ranging from a mere 5 milligrams to 700 milligrams, the largest amount ever given in a cancer study. Even at the highest dose, there were few negative side effects other than fatigue (fifteen patients) and mild nausea or diarrhea (eight patients). But the effect on tumor growth was marginal, which has been true in every study in which melatonin is used as a solo agent. Six of the forty-two patients showed a significant reduction in tumor size. Six more had a stable condition, which means that their tumors neither grew nor shrank. Clearly, melatonin alone is not a magic bullet against cancer.
-
Nonetheless, a few of the patients did quite well with the treatment, two of them being women with brain metastases. Brain tumors are notoriously difficult to treat because most cancer drugs have difficulty crossing the blood-brain barrier. As you recall, melatonin does not share this limitation. One of the women who had the most dramatic response was eighty-three years old. Prior to taking part in the study, she had been treated with radiation and interferon (another experimental therapy). Neither treatment had worked, and the melanoma had invaded her brain. She was given a 50-milligram dose of melatonin in tablet form every four hours, a treatment that was without significant side effects; she suffered no nausea or hair loss and no damage to her immune system, heart, liver, or other organs. Amazingly, at the end of eight months, she had an “almost total regression of her disease. “29
· Chapter 7 - Protecting Your Heart
page 85:
- Antioxidants reduce the oxidation of LDL cholesterol and prevent it from adhering to artery walls.
page 86:
- In 1975 a researcher discovered that if he gave melatonin to pinealectomized animals, their blood pressure went down—in some instances to below normal levels. When he stopped giving them melatonin, their blood pressure shot back up, indicating a cause-and-effect relationship between blood pressure and melatonin.22
page 89:
-
How does melatonin affect blood pressure? There are three possible mechanisms. One is that the hormone acts directly on the hypothalamus, an area deep in the brain that regulates blood pressure and is known to be rich with melatonin receptors. Another and more recent explanation is that melatonin lowers blood pressure through its antioxidant effects. Several studies have shown that antioxidants lower blood pressure. 29 Interestingly, they seem to have a marked effect only in people with hypertension, and the same may be true for melatonin. When Birau gave the melatonin nose drops to people without hypertension, their blood pressure remained essentially unchanged. Finally, melatonin may link with receptors on arterial walls, causing the arteries to expand. This third possible mechanism was presented by L. Bruce Weekley, Ph.D., in The Journal of Pineal Research. in 1991. In a study of rats, Weekley found that melatonin relaxes the smooth muscle lining the aorta.30
-
How do Antioxidants Lower Blood Pressure?
-
The blood vessels are lined with a layer of endothelial cells that secrete relaxing factors, which cause the vessels to expand, thus lowering blood pressure. One such relaxing factor is nitric oxide. Nitric oxide is rapidly inactivated by a free radical called the superoxide radical. Increasing your antioxidant protection reduces the number of superoxide radicals, which spares nitric oxide and allows the blood vessels to expand. The net result is lower blood pressure.
page 90:
-
If you are currently taking anti-hypertensive medication, however, you should continue doing so. The medication may be preventing a heart attack or stroke. There is no evidence at this time that melatonin can replace traditional heart medications. The data is merely suggestive.
-
As of 2024, several trials have show melatonin to be effective in controlling high blood pressure. See: https://doi.org/10.2147/JMDH.S446521
-
Platelets are small cell fragments that are formed in the bone marrow and that circulate throughout the bloodstream to help guard against the loss of blood. When a blood vessel is injured, platelets clump together to help seal the breach. A careful balance must be maintained, however. If your platelets become too sticky, they may clump together unnecessarily and block a vital artery; if they become too slick, they will no longer function as a Band-Aid, and you might run the risk of uncontrolled bleeding. Your body has worked out a clever compromise between these alternatives. During the daytime, when your risk of physical injury is highest, your platelets are more likely to clump together. When you are safely tucked away in bed, your platelets are less sticky, lowering your risk of heart attack and stroke without putting you at undue risk. There is reason to believe that this compromise is mediated by your nocturnal rise in melatonin. When human blood platelets are incubated in a melatonin solution, the hormone reduces their tendency to clump by as much as 85 percent.33
page 91:
-
Anytime that blood is blocked from your heart and then flows back in, free radicals are produced, which cause some amount of tissue damage. To minimize this damage, heart specialists have begun to give antioxidants to their patients before surgery, and a growing number of hospitals are adding antioxidants to the blood supply before transfusing it into a heart patient.
-
The higher the electrical stability of the heart, the less likely the current will cause arrhythmia. In the Harvard study, researchers gave injections of melatonin to a group of dogs, then measured the amount of current required to destabilize their hearts. The melatonin-treated dogs required 28 percent more current than dogs not given the heart-calming hormone. 36
-
They made another interesting observation: There is a high incidence of arrhythmias in patients admitted to intensive care units (ICUs), even when the patients do not have preexisting heart problems. Knowing that bright light can inhibit the body’s production of melatonin (a topic 1 will explore in Chapter 13), the researchers speculated that the continuous lighting in ICUs might lower patients’ melatonin levels, thereby reducing the electrical stability of their hearts and making them more vulnerable to arrhythmia.
· Chapter 8 - Unlocking the Sleep Gate
page 94:
- In the United States approximately one out of every four adults and two out of every four senior citizens have trouble falling asleep or staying asleep.
page 100:
- Another reason that melatonin is such a superlative sleep aid is that it does not lose its effectiveness over time. Benzodiazepines can become less effective after only two or three nights of use. By contrast, melatonin may become a more effective sleep aid with chronic use. In an Israeli study, researchers gave 2-milligram doses of melatonin to elderly volunteers for two months. At the end of the treatment period, the volunteers fell asleep even more quickly than they did after one week of treatment. 19
page 103:
-
You feel less tense, your reaction time slows, your pulse rate declines, you feel a sense of tranquillity, your body temperature drops, and you begin to feel sleepy. These multiple changes are referred to as “opening the sleep gate." Once the gate is open, it is much easier to fall asleep.
-
Melatonin’s effect on body temperature is one of the keys to its ability to enhance sleep. It has been known since 1835 that the temperature of the human body has a distinct circadian rhythm, rising during the day and falling at night. The daily swing in temperature is only about a degree, but it still has a strong influence on sleep. As a rule, it is easier to fall asleep when your body temperature is falling and to wake up when it is on the rise. Interestingly, you will fall asleep the most quickly and sleep the longest if you turn out the lights while your body temperature is dropping the most rapidly.27 This fall happens to coincide with the steepest rise in your nightly melatonin levels, which takes place somewhere between nine P.M. and twelve a.m., depending on your unique circadian rhythm. If you go to bed at some other point in your melatonin cycle, either earlier or later, your sleep may be neither as restful nor as long.
-
studies have shown that melatonin has a direct effect on body temperature. Researchers have found that if you take a melatonin tablet during the daytime, when your natural melatonin levels are low and your body temperature is high, it will lower your temperature. Conversely, if you block your melatonin production at night by exposing yourself to very bright light or by taking a melatonin- lowering drug such as a beta-blocker, your body temperature will rise.
page 104:
-
You can also change your melatonin levels by changing your body temperature. In one study, volunteers sitting in a hot bath in the middle of the day experienced about a two-degree rise in body temperature. Blood samples drawn from them showed an accompanying rise in their pielatonin level. Sitting in a lukewarm bath, however, produced no rise in body temperature or in melatonin level. This effect may be why taking a hot bath or shower at night helps you fall asleep more quickly: The hot water raises your body temperature, which causes your pineal gland to produce melatonin—perhaps in an effort to maintain a stable temperature. The melatonin causes your temperature to drop back down, swinging open the sleep gate and welcoming you into the land of Nod. 28
-
The preliminary data from this study shows that melatonin is just as effective as temazepam in reducing the amount of time it takes the subjects to fall asleep. It also extends sleep the same amount of time. But unlike temazepam, melatonin does not delay REM sleep, and therefore it results in a more normal sleep architecture.29
page 107:
- Very small amounts of melatonin—0.2 milligrams in a time-release pill—increased the total sleep time of some Alzheimer’s patients by as much as two hours—a remarkable improvement for such a low dose. The patients who responded the best were those who had had the most trouble sleeping. A more comprehensive study is now under way, using 0.5 milligrams.
page 108:
-
it (Melatonin) may not be effective for people kept awake by moderate to severe pain, marked anxiety, or deep depression.
-
pilot study to see if combining melatonin with a benzodiazepine will help people with anxiety-related sleep problems. Preliminary results suggest that in normal subjects, this combination produces a more restful sleep than benzodiazepines alone.
-
Some people with fibromyalgia find that melatonin alone solves their sleep problems. Billie Sahley, Ph.D., the founder of the Pain and Stress Center in San Antonio, has recommended melatonin to a number of patients with this condition. She says, “They take three milligrams at bedtime, and they sleep much better. They also experience less pain.” But other people with this condition require additional medications as well. (Amitryptyline plus melatonin is a frequently used combination.)
· Chapter 9 - Back in Sync
page 110:
- The term body clock refers to a tiny bundle of nerves called the suprachiasmatic nuclei, or SCN,’ located in the brain directly behind the eyes. The nerve cells of the SCN transmit chemical messages on a regular schedule, approximately twelve hours “on” and twelve hours “off.” (The total duration of the cycle is about twenty-five hours.) This built-in rhythm is unique to SCN cells.
page 111:
-
the SCN signals the pineal gland to produce a hormone that can be sent into the circulatory system, which is a communication network that does, in fact, reach every cell. That hormone is melatonin.
-
The signal from the SCN releases a neurotransmitter called norepinephrine, which stimulates pineal cells to produce melatonin. No signal, no norepinephrine; no norepinephrine, no melatonin.
-
When light from the sun (or some other bright light source) shines in the eyes, a message is sent down the pathway to the body clock, switching it to the “off” phase.
-
About twelve hours later, the body clock turns itself back on, the signal for the pineal gland to resume production.
page 112:
- If you work the night shift or fly across time zones, your body clock is likely to adjust, but it may take about a day for each hour your schedule is shifted.
page 116:
- As a rule, it’s easier to adapt when you fly west. Your body clock actually operates on about a twenty-fife-hour schedule. Flying west demands that you stretch out your day, going to bed later than you did in your hometown. Your native twenty-five-hour cycle helps you stay up later than normal. Flying east, however, demands that you compress your daily schedule, taking away this built-in advantage.
· Chapter 10 - A Master Sex Hormone
page 121:
- Our first task was to remove the pineal glands from a group of ham- sters. It was tricky because the gland is no bigger than the period at the end of this sentence. We had to use an operating microscope to perform the operation. When the animals recovered from the surgery, we put them in the hibernating dens. To have a basis for comparison, we included a group of animals that still had their pineal glands. Then we waited. After about two weeks, Hoffman suggested that we examine the animals. He was like a kid who couldn’t wait until Christmas. 1 persuaded him to hold off a little longer. Finally, after four weeks, we opened the cages and got our first good look at the animals. The difference between the two groups was remarkable. The animals with pineal glands had shriveled-up gonads—the expected response to the environmental conditions. But the animals without pineal glands were flaunting regulation-size-and-weight testicles. Some substance produced by a little dot of a gland could apparently cause a sixfold difference in the size of the animals’ testes.1
page 122:
- After many years of frustration, we finally were able to prove that our assumption was correct. Melatonin was indeed the chastity hormone.
page 123:
-
Now we know that this annual cycle of melatonin production sets in motion a host of other seasonal changes in animals as well, including changes in the color and thickness of their coats, the sprouting of antlers, and the annual migration. To everything there is a season—thanks, in part, to melatonin.
-
If you look very closely, you can see remnants of a seasonal breeding cycle in humans. In Seattle, for example, more twins are conceived in the summer months than in the winter months. According to the investigators, the increased hours of daylight “may stimulate multiple ovulation.“2
page 124:
-
This seasonal effect becomes more pronounced the farther north you go. In northern Finland, which is above the Arctic Circle, there is an eight-week period in the summer in which the sun never sets. During this long period of continuous light, the rate of conception increases significantly.
-
Finnish researchers measured the nocturnal melatonin production of a large group of women from northern Finland in the summer and winter. They found that the women had significantly lower levels of the hormone in the summer months.3
page 125:
- Although this idea has not been confirmed, high levels of melatonin are associated with infertility in women.
page 126:
- Michael Cohen, the developer of the B-Oval contraceptive pill, has had a long-standing interest in melatonin’s effects on female reproduction. Noting that a high level of melatonin inhibits ovulation in animals, he wondered if the same was true in women. In a series of pilot studies, he gave women various doses of melatonin. When melatonin was packaged in a slow-release format (extending the amount of time that it remained in the bloodstream), doses as low as 10 milligrams inhibited ovulation in some of the women some of the time. To produce a reliable birth control pill, however, he had to increase the dose of melatonin to 75 milligrams and then combine it with 0.3 milligrams of a progestin called norethisterone (NET).
page 127:
-
Studies have shown that women with PMS produce less melatonin than other women, especially in the week before menstruation, when women without this syndrome have a pronounced luteal surge. This happens to be the very time when symptoms of PMS are most evident. 10
-
Relief from PMS is one of the many benefits reported by women taking the B-Oval pill. This reaction is so consistent among Cohen’s study population that he has developed a melatonin-based treatment for PMS. In his patent application for the new medication, Cohen states, “It has been found that the administration of melatonin to women, preferably during the luteal phase of their cycles, leads to a substantial reduction in, and in some instances, the disappearance of, the symptoms of PMS.“11
-
Meanwhile, Dr. Sarafina Corsella, a New York psychiatrist who practices holistic medicine, has gotten excellent results treating PMS patients with melatonin. She recommends a dose of 1 or 2 milligrams (taken at night) starting at midcycle and then extending until menstruation. She augments the melatonin with a natural progesterone cream, the amount of progesterone depending on the patient’s individual hormonal profile.
page 129:
-
A paper published by an Israeli group in 1995 showed that giving melatonin on a nightly basis to aging rats prevented the age-related decline in testosterone production. In fact, the melatonin-treated rats had almost three times as much testosterone as those not given the hormone. 20
-
Another way that melatonin may enhance male sexuality is by increasing the firmness and frequency of erections.
-
Finally, melatonin may enhance the motility or forward movement of sperm.
· Chapter 11 - Melatonin and Your Mind
page 134:
- Lithium, a drug commonly prescribed for bipolar disorder, is yet another melatonin enhancer.8
page 135:
-
Depression has also been relieved by taking tryptophan, the amino acid from which melatonin is derived. Taking tryptophan has been shown to increase melatonin levels. 11 In a number of studies involving tryptophan, the relief of depression corresponded with an increase in melatonin production. 12
-
In recent years it has been discovered that Saint-John’s-wort (Hypericum), a common groundcover plant, raises melatonin levels. 13 Saint-John’s-wort has been used as a folk remedy for depression for more than two thousand years. Rigorous scientific studies have shown that the herb does indeed have a significant antidepressant effect, yet another substance that relieves depression and also stimulates melatonin production.
page 136:
-
Today pharmaceutical companies are investing billions of dollars in researching the antidepressant properties of melatonin’s close cousin, serotonin, the neurotransmitter that is enhanced by drugs such as Prozac and Zoloft. In some respects, melatonin is a more logical candidate as a treatment for depression. Serotonin has difficulty crossing the blood-brain barrier. Therefore, to increase the activity of serotonin in the brain, pharmacologists have to concoct drugs that block the enzymatic destruction of the compound or prevent it from being reabsorbed by neurons. But to increase melatonin levels in your brain, all you have to do is take melatonin. Given the preliminary evidence that melatonin may enhance mood in some people, coupled with its apparent lack of toxicity and negative side effects, it is reasonable to suggest that a few million dollars might be diverted to exploring the antidepressant potential of melatonin.
-
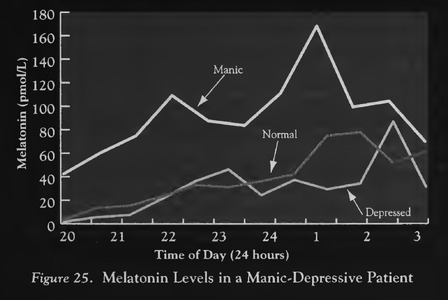
People who suffer from manic depression, or bipolar mood disorder, are troubled by mood swings that can careen from euphoria to despondency. There is some evidence that their melatonin levels go along on the roller-coaster ride, peaking during periods of mania and plummeting during periods of depression.
page 137:
- Canadian psychiatrists provided further insight by measuring the melatonin levels of one patient in all three phases of the illness. They drew blood samples from the twenty-nine-year-old woman at three separate occasions: when she was manic, when she was depressed, and when she was feeling normal. They found she was producing more than twice as much melatonin when she was manic than when she was depressed. When she was symptom free, she had normal amounts of the hormone.18 In this instance, there was a clear correlation between melatonin levels and mood.
page 138:
-
chronic pain sufferers in their study had low levels of melatonin compared with the controls. Patients with nerve-related pain had the lowest levels of all.22
-
What is most intriguing to me about the relationship between melatonin and chronic pain is that melatonin has potent analgesic properties, suggesting a cause-and-effect relationship between low melatonin levels and pain.
-
A group of researchers from the University of California became interested in the possible pain-relieving properties of melatonin when they noted that many animals are less sensitive to pain at night. This is true for both nocturnal and diurnal animals. In one experiment, they placed mice on a very warm surface and observed how long it took them to show signs of discomfort. It took an average of 62 seconds in the daytime but 110 seconds at night, indicating that the mice had a higher tolerance for pain at night. Other studies had shown that mice are most tolerant of pain shortly after midnight, which is when they have the highest levels of melatonin.
-
The California researchers’ next step was to give rodents varying amounts of melatonin to see if added amounts of the hormone increased their pain tolerance. They found that the more melatonin they gave the rodents, the longer they were willing to stay on the hot surface. At the highest dose (90 milligrams per kilogram) of melatonin, the mice tolerated moderate pain three times as long as they did without melatonin. In fact, dose per dose, melatonin was almost as effective at relieving pain as morphine. 23
page 140:
- former alcoholics were producing much less melatonin than members of a control group who did not have a history of alcoholism.
page 141:
-
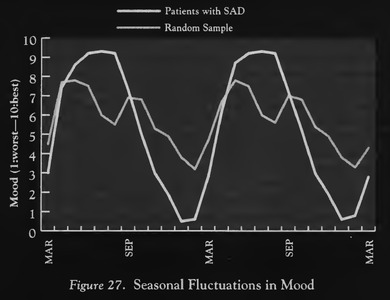
Many of the symptoms of SAD are quite different from the symptoms of nonseasonal depression. People with nonseasonal depression tend to complain of a lack of appetite, insomnia, low self-esteem, and feelings of helplessness or hopelessness. SAD sufferers have a different litany of woes. They are troubled by sleepiness, low energy, social withdrawal, and increased appetite—especially for sweets and other carbohydrates.
-
If you stop to think about it, the symptoms of SAD sound a lot like those of hibernation. Hibernating animals stock up on food in the fall and then climb into a dark hole and sleep out the winter. It doesn’t take too much imagination to reframe these behaviors as carbohydrate craving, fatigue, and social withdrawal.
· Chapter 12 - The Great Anti-Aging Experiment
page 147:
- when the mice that were drinking plain water began to die one by one, right on schedule, while the melatonin-treated mice continued to thrive. When the last mouse had died, the researchers discovered that the average survival time of the water-drinking mice was 752 days, typical for this strain of mouse, but the mice that had been given the melatonin nightcaps had lived an average of 931 days—a 20 percent increase in lifespan.2
page 151:
-
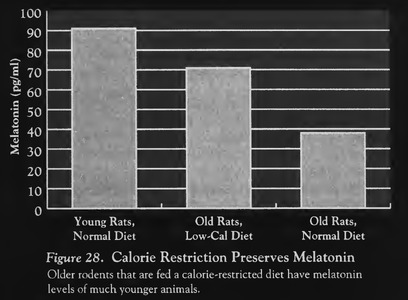
other anti-aging strategies. The most effective and well-researched strategy is calorie restriction If young animals are limited to 60 percent of their normal food intake, they live as much as 50 percent longer than animals given free access to food. In addition, the animals have a lower incidence of virtually all degenerative diseases and appear more youthful well into old age.
-
This suggests that calorie restriction and preserved melatonin production go hand in hand.
page 153:
- A French study conducted in 1985 compared the melatonin levels of 757 hospitalized male and female patients and discovered that the women produced an average of 25 percent more melatonin than the men.12 A second study, this one a multinational study conducted by Swedish researcher Lennart Wetterberg and published in 1993, surveyed 321 healthy individuals and found that the women produced approximately 20 percent more melatonin than the men, even though, on average, the women had less body mass. A third study of 102 people revealed that women produced 30 percent more of the life-giving hormone than men.‘13 Finally, a German study of 174 subjects detected higher levels of melatonin in older women compared with older men.14
page 154:
- The healthy elderly were producing more than twice as much melatonin as Alzheimer’s patients of a similar age.18
Part 2 - Attaining Healthy Levels of Melatonin
· Chapter 13 - Let There Be Light And Dark
page 160:
- two groups and came up with a significant finding: The rats in the sunlit room were producing far more melatonin at night than the ones in the artificial lighting environment.1
page 164:
-
serotonin, melatonin’s parent molecule.
-
A high level of serotonin during the day punctuated by a strong pulse of melatonin at night appears to be nature’s formula for vibrant good health. Serotonin keeps you alert and energized during the daytime; melatonin helps you rest and recuperate at night.
page 165:
- We would do well to heed some ancient teachings. The Tao Tsang, a two’thousand-year-old Chinese text, teaches that “exposing the eyes to direct sunlight greatly benefits the brain by stimulating secretions of vital essences there."‘11 We happen to call those vital essences melatonin and serotonin, but my guess is that the Chinese sages were describing the same phenomena. The yogic tradition maintains that the pineal gland is the “crown chakra” through which solar radiation energizes the body.‘12 The Bible proclaims, “The lamp of the body is the eye. If your eyes are sound, you will have light for your whole body, if the eyes are bad, your whole body will be in darkness” (Matthew 6:22-23).
page 166:
-
In one study, 500 lux of light suppressed melatonin production by 8 percent in one person but an amazing 98 percent in another. 14 There is some indication that people with low levels of melatonin are most vulnerable to the suppressive effect of light. 15
-
Another group of people who may be especially sensitive to light exposure are those who take extra vitamin B-12 (more than the recommended daily requirement). High amounts of this particular vitamin can cause melatonin production to drop more dramatically in response to light at night and take longer to recover once the light is turned off.16
-
How long must you be exposed to bright light at night before your melatonin production is inhibited? As little as five minutes, according to a 1989 study. 17 To my knowledge no one has studied the effects of a shorter exposure. In some laboratory rats, a one-second pulse of light is enough to lower their melatonin levels, but it is generally agreed that people are far less sensitive.
-
By itself, being awake does not shut down melatonin production. If you were to lie wide awake at night in a dark room, you would produce just as much melatonin as if you were sound asleep.
· Chapter 14 - The Elusive Enemy- Electromagnetic Fields
page 175:
-
magnetic fields interfere with melatonin’s ability to slow the growth of breast cancer cells,
-
Other researchers had found that EMFs may lower the amount of melatonin in the bloodstream; Liburdy found that EMFs may block melatonin’s actions. This implies that even if you have adequate amounts of melatonin—or take melatonin supplements—EMFs may render the hormone impotent, depriving you of its anticancer action.
· Chapter 15 - Drugs That Deplete Melatonin
page 182:
-
Volunteers who took just one normal dose of aspirin or ibuprofen in the evening had as much as a 75 percent reduction in melatonin levels.1
-
Many arthritis sufferers rely on these drugs extensively to cope with their pain. What options do they have? Dr. Billie Sahley at the Pain and Stress Center in San Antonio recommends melatonin itself to arthritis sufferers. “So far we’ve seen excellent results. They are reporting a remarkable decrease in pain.”
page 186:
- At least two widely prescribed anti-anxiety drugs, diazepam (Valium) and alprazolam (Xanax 16) inhibit melatonin production.17
page 187:
-
In a 1992 ‘Japanese study, nine healthy men were given three daily doses of vitamin B-12 for a total of 3 milligrams a day. Compared with the placebo, vitamin B-12 caused a significant decrease in their average twenty-four-hour melatonin levels.23 (Vitamin B-12 is contained in most multivitamin preparations, but usually in such small doses that it is un- likely to influence melatonin production.)
-
Bowling Green State University measured the melatonin levels of a group of individuals who volunteered to stay awake for two consecutive days. Some were given a placebo and others were given 200 milligrams o{ caffeine, which is equivalent to two cups of strong coffee. (Eight ounces of instant coffee contains approximately 65 milligrams of caffeine. Freshly brewed coffee ranges from 75 to 120 milligrams.) Compared with the placebo, caffeine caused a significant” reduction in their melatonin levels.24
page 190:
-
(The steroid) Dexamethasone also reduces melatonin levels.
-
equivalent of one or two glasses of wine at seven o’clock in the evening had 41 percent less melatonin at midnight
-
When they were given higher doses of alcohol, they had low melatonin levels until the early hours of the morning.33
page 191:
- SUBSTANCES THAT MAY DECREASE MELATONIN Acetaminophen Alcohol Alprazolam Aspirin Atenolol Benzerazide Bepridil Caffeine (coffee, tea, and some soda drinks) Clonidine Dexamethasone Diazepam Diltiazem Filodipine Flunitrazepam Fluoxetine Ibuprofen Indomethacin Interleuken-2 Isradapine Luzindole Methylcobalamine Metoprolol Nicotine Nicardipine Nifedipine Nimodipine Nisoldipine Nitrendipine Prazosin Propranolol Reserpine Ridazolol Tobacco Vitamin B-12
· Chapter 16 - Creating a Melatonin Friendly Lifestyle
page 192:
-
Thy food shall be thy medicine. —Hippocrates (460-377 B.C.)
-
A truly good physician first finds out the cause of the illness, and having found that, he first tries to cure it by food. Only when food fails does he prescribe medication. —Sun Ssu-Mo, Tang Dynasty (a.d. 600)
-
Normal resistance to disease never comes out of pill boxes. Adequate food is the cradle of normal resistance, the playground of normal immunity, the workshop of good health, and the laboratory of long life. —Charles Mayo, founder of the Mayo Clinic (1915)
page 194:
- another way to raise your melatonin levels—take tryptophan
page 197:
- It is not known precisely which amounts of the vitamins and minerals I’ve mentioned produce optimum levels of melatonin, although a study that is now under way may provide the answer. But for the present you might start with 100 milligrams of niacinamide, 25 to 50 milligrams of vitamin B-6, 1,000 milligrams of calcium, and 500 milligrams of magnesium.9 Ask your physician if there is any reason you should not be taking these supplements in these amounts. What time of day should you take these supplements? Take the niacinamide, calcium, and magnesium just before going to bed. However, the B-6 should be taken early in the day because it may make you feel more alert and energized, interfering with your sleep.
page 198:
- Of all the known ways to stimulate melatonin production, none is more dramatic than smoking marijuana. Marijuana stimulates production of a prostaglandin called PGE2, which may relate to its ability to stimulate melatonin production. Italian researchers discovered that when eight men smoked a cigarette containing the active ingredient in marijuana, THC (tetrahydrocannabinol), they had dramatically higher melatonin levels twenty minutes later. After two hours, their melatonin levels were 4,000 percent higher than at baseline!‘11
· Chapter 17 - Taking Melatonin Supplements
page 201:
-
If you are 60 or older, for example, creating a melatonin-friendly lifestyle may not be sufficient to restore your youthful supply of the hormone.
-
People 70 and older may produce less melatonin at night than young people do in the daytime.
page 205:
-
People taking steroid drugs such as cortisone and dexamethasone (should avoid melatonin) since Melatonin may counteract the effect o{ these medications.9
-
People with severe allergies (should avoid melatonin) since Melatonin stimulates the immune system and could exaggerate an allergic response.13
-
People with autoimmune diseases (should avoid melatonin) since Melatonin stimulates the immune system and could exaggerate an autoimmune response.14
-
People with immune-system cancers such as lymphoma and leukemia (should avoid melatonin) since elatonin may further stimulate the immune cells. 15
page 206:
- A very few people seem to have atypical reactions to taking melatonin. They may have insomnia, nightmares, or dream so vividly that they feel as if they’re not sleeping.
page 208:
- Most tablets and gelatin capsules are regarded as “fast-release” preparations because no steps have been taken to slow down the rate of absorption. When you swallow a fast-release preparation, it goes to your stomach, where it is broken down into smaller fragments. It then passes from the stomach into blood vessels in the wall of your stomach; this blood is then filtered through the liver. The liver metabolizes a high percentage of the melatonin, converting it into a substance called 6-hydroxymelatonin sulfate, which is then excreted in the urine. 19 (This process is called a first-pass effect, because it is the first time melatonin is presented to the liver.) The amount metabolized on this first pass varies greatly from person to person. A person with an efficient liver may metabolize most of the melatonin,’ preventing 95 percent of it from entering the general circulation. A person with a less efficient liver may experience a minor first-pass effect, allowing much greater amounts to enter the bloodstream. One study of five individuals found a thirty-five-fold difference in the amount of melatonin in the serum following ingestion of the same 2-milligram dose.20
Part 3 - The Future of Melatonin Research
· Chapter 18 - When God Holds the Patent
page 221:
- Ferdinando Anton-Tay was the first clinician to administer melatonin to epileptic patients. In 1971 he gave melatonin injections to three epileptic patients. He monitored the brain waves of the patients before and after administering the hormone and found that melatonin normalized their brain waves, particularly during the first four hours after administration.6 He continued to give melatonin to one of the patients for two additional days, during which time the patient was seizure free, despite the fact that his other medications had been withdrawn.7
page 222:
- But the link between SIDS and the pineal gland is more than a theory. Larry Sparks, Ph.D., associate professor of neurology and pathology at the University of Kentucky, has examined the pineal glands of more than a hundred SIDS babies. He reports that in all but a few instances, the glands were small and abnormal in appearance. 10
page 224:
-
Diabetes is a deadly disease. Fifty percent of people diagnosed with insulin-dependent (type I) diabetes before the age of 30 are dead by age 50. Diabetes is also the leading cause of new cases of blindness and is a contributing factor in 50 percent of all heart attacks and an even higher percentage of all strokes.
-
It was reported in 1986 that people with diabetes may have abnormally low levels of melatonin. An English team headed by Josephine Arendt compared the nocturnal melatonin levels of sixteen diabetics with a group of age-matched healthy volunteers. The diabetics were producing significantly less melatonin. In fact, five of the sixteen diabetics had barely detectable amounts of the hormone. Diabetics with an accompanying nerve disorder called autonomic neuropathy had a flip-flopped circadian rhythm, producing more melatonin during the day than at night. 14
-
Low melatonin levels could contribute to a number of health problems common to diabetics. Many diabetics have sleep difficulties, for example. In one study, 33 percent of a group of diabetics had severe sleep problems, compared with only 8 percent of an age-matched group of nondiabetics.15 Diabetics also have a high incidence of cataracts, hypertension, high cholesterol, infections, and stroke—diseases that may be caused or exacerbated by free radicals. 16 An inadequate supply of antioxidants is likely to increase the risk of being afflicted by these particular conditions.
page 226:
- no pharmaceutical company has shown a great interest in melatonin research because the molecule cannot be patented.
page 227:
- Instead of investigating melatonin itself, pharmaceutical companies are fabricating “analogues” of melatonin, molecular look-alikes that hopefully share some of the properties of the hormone but are different enough in molecular structure to qualify for a patent. To date, more than a hundred melatonin analogues have been patented.20