Home · Articles · 2024 · Ketogenic Diet for T1 Diabetes Notes
My notes highlighted in light blue
- Dr. Bernstein’s Diabetes Solution: The Complete Guide to Achieving Normal Blood Sugars
If you aren’t opposed to piracy, I’ve hosted a copy here.
1. Ketogenic diets in the management of type 1 diabetes: Safe or safety concern?
source:: https://www.ccjm.org/content/88/10/547
1.1. CASE CONCLUSION
Two years after starting the ketogenic diet, the patient reported that his blood glucose control remained significantly improved. His HbA1c level has remained in the desired range for the past 2 years; most recently it was 5.5%. He lost 35 lbs with BMI improved from 30.4 to 25.5 kg/m2. His total average daily basal insulin requirement decreased from 48 to 30 units per day, and he reported that he rarely requires prandial or correctional insulin boluses (before the diet, he averaged 33 units per day). According to his pump and CGM download, his bolus insulin requirements comprised only 3% of his total daily insulin dose (average of 1 unit per day). His blood glucose level remained within the goal range (3.9−10.0 mmol/L [70−180 mg/dL]) 98% of the time. He reported episodes of hypoglycemia 2 to 3 times every 2 weeks, but these have been mild and easily manageable. He has not had any episodes of DKA or severe hypoglycemia since starting the diet, but also admitted he would not feel safe following the diet without the safety afforded by CGM. He experienced an increase in low-density lipoprotein level up to 221 mg/dL, requiring starting high-dose atorvastatin, which may be due to a high proportion of saturated animal fats in his diet. He responded well to statin therapy and his low-density lipoprotein level decreased to 104 mg/dL, which has been maintained on the therapy.
1.2. THE BOTTOM LINE
Further research is needed on the efficacy and safety of the ketogenic diet in patients with type 1 diabetes. The diet may be appropriate for select patients, but only after a thorough discussion between patient and care team about the risks and benefits. A registered dietitian and specialists in diabetes care, education, endocrinology, and pharmacy should be part of any discussion. For patients on the diet, extra monitoring is critical, preferably with a CGM.
2. Nutritional ketosis is well-tolerated, even in type 1 diabetes: the ZeroFive100 Project; a proof-of-concept study
source:: https://pubmed.ncbi.nlm.nih.gov/34334612/
Recent findings: Eight adults, ages 28-62 years, trained for and completed a 5-day zero calorie fast covering 100 miles over 5 days. Training involved each individual preparing for the event according to their own programme. Typically, it involved both cardiovascular and strength training with the addition of practice water only fasts over 24-72 h or more based upon the individual’s assessment of what was needed to complete the event. There was no formal protocol provided for this. The recommendation was that the participants would be keto adapted and trained to a level sufficient to complete the 5-day event. Keto adaptation was measured by ketone blood testing of betahydroxybutyrate. Two people had type 1 diabetes. All but one person was keto-adapted ahead of the event. All eight individuals completed the project with no physical injuries or problems with diabetes control. Prolonged fasting did neither lead to hunger nor did it negatively affect mood, which, if anything, was enhanced in most individuals. All keto-adapted people were shown to be burning fat stores throughout the 5 days, and everyone was measured to be in a state of nutritional ketosis. In type 1 diabetes, and ketones were in the same range as those without diabetes, insulin volumes were considerably reduced, and glucose control was close to physiological: nutritional ketosis is not a risk factor for diabetic ketoacidosis; consumption of sugar for energy is not required for distances of up to 100 miles in keto-adapted people; people who inject insulin do not necessarily need to consume carbohydrates unless rescuing a hypoglycaemic attack.
Summary: The findings from this project should provide reassurance to those clinicians who want to provide the option of a ketogenic lifestyle to their patients with type 1 diabetes. They also confirm that the fat stores are available for aerobic respiration without apparent negative consequences on physical or mental function.
3. The glycaemic benefits of a very-low-carbohydrate ketogenic diet in adults with Type 1 diabetes mellitus may be opposed by increased hypoglycaemia risk and dyslipidaemia
source:: https://onlinelibrary.wiley.com/doi/10.1111/dme.13663
3.1. Results
The mean ± sd HbA1c levels were 35±4 mmol/mol (5.3±0.4%), and participants spent 74±20 and 3±8% of their time in the euglycaemic (4–8 mmol/l) and hyperglycaemic (>10 mmol/l) ranges, respectively, with little daily glycaemic variability (sd 1.5±0.7 mmol/l; coefficient of variation 26±8%). Blood glucose levels were <3.0 mmol/l for 3.6% of the time, and participants experienced a median (range) of 0.9 (0.0–2.0) daily episodes of hypoglycaemia. Total cholesterol, LDL cholesterol, total cholesterol/HDL cholesterol ratio, and triglycerides were above the recommended range in 82%, 82%, 64% and 27% of participants, respectively; however, HDL cholesterol levels were within the recommended range for all participants. Participants displayed no or little evidence of hepatic or renal dysfunction.
Again, I think high LDL is only a problem if you have deficiency in sulfur.
3.2. Conclusion
This study provides the first evidence that, ketogenic diets in adults with Type 1 diabetes are associated with excellent HbA1c levels and little glycaemic variability, but may also be associated with dyslipidaemia and a high number of hypoglycaemic episodes.
4. Ketogenic diet and type 1 diabetes
source:: https://medium.com/@andreiatorres/ketogenic-diet-and-type-1-diabetes-43b9e981cdbd
Interview with German nutritionist that has T1.
5. Type 1 Diabetes and The Ketogenic Diet: Benefits & Risks
source:: https://www.ruled.me/type-1-diabetes-ketogenic-diet/
Again, if not opposed to piracy, I have hosted a copy of the study here.
The young girl in the first case study had epilepsy and type 1 diabetes, which is more prevalent in children with epilepsy. Researchers sought after an effective diet for this complicated case, so they put the girl on a classic ketogenic diet (about 5% daily calories from carbs and 75% from fat) for 15 months.
The results were promising. Since the start of the ketogenic diet, no clinically overt seizures were reported. The girl was even being much more active and reaching significant developmental achievements that she wasn’t reaching before the ketogenic diet.
The researchers also tracked the girl’s A1C levels and glycemic control, the two most important measures for type 1 diabetics. Both of them improved significantly without any adverse side effects. These results indicate that the ketogenic diet may help manage type 1 diabetes and epilepsy simultaneously.
The results of the other case study were even more incredible. In the study, a 19-year-old male with newly diagnosed type 1 diabetes was put on a special type of ketogenic diet for 6.5 months. During this period, he was able to discontinue insulin use and restore some of the insulin production in his pancreas.
The researchers went on to conclude that:
…an intervention with the paleolithic ketogenic diet in an early stage of the disease with residual insulin secretion may halt or reverse type 1 diabetes mellitus. Follow-up at sixth month in the case of our patient is relatively short and the positive results may appear as a honeymoon effect.
The honeymoon effect is the period of time when the pancreas is still producing enough insulin to aid blood glucose control. Because of the honeymoon effect, it is much more likely that the paleolithic ketogenic diet didn’t halt or reverse type 1 diabetes. However, the possibility that this diet is responsible for this patient’s incredible recovery still remains.
To get a more definitive understanding of these results, I reached out to the authors of the case study for an update on their patient’s condition. One of the researchers responded promptly with this:
No, it was not a honeymoon period. But he decided to stop the diet and therefore had to go back to insulin. Another patient with a much longer follow-up: Case Study
Although this indicates that type 1 diabetes was not reversed (in both cases), these results are still impressive — and the paleolithic ketogenic diet is the primary reason why.
But what exactly do the researchers mean by a “paleolithic ketogenic diet”?
Here’s how they described it:
His diet consisted of meat, organ meat, fat, and eggs. In his diet, red and fat meats dominated over lean meats. He was eating vegetables in insignificant amounts. His diet had a ketogenic ratio (fat:protein + carbohydrate) of at least 2:1. No oil of plant origin or artificial sweeteners were allowed.
He also took 5,000 IU of vitamin D3 and excluded all milk and dairy from his diet [two important dietary strategies that we will address later].
The best part is that it didn’t take six months for the combination of the paleolithic ketogenic diet with vitamin D supplementation to produce results. In fact, the tapering of insulin was done promptly. Researchers stated that following the first paleolithic-ketogenic meal glucose level was only 86 mg/dL thus there was no need for external insulin.”
However, there is some bad news. These case studies only reflect what happened to one young girl and one adolescent male on a ketogenic type diet. This means that these results may not apply to other type 1 diabetics. We need some evidence from larger studies as well. Luckily, there are two.
In one study consisting of twenty-two patients with type 1 diabetes, carbohydrate restriction was put to the test. While they were on a diet that limited them to 70-90 g carbs per day, participants had significantly less hypoglycemic (low blood sugar) episodes, lower A1C levels, and required less insulin after three months of carbohydrate restriction.
A similar result was found in another study on 48 people who had type 1 diabetes for 12 years or longer. They were simply educated on how to reduce carbohydrate consumption and lower their insulin dosages. Twenty-three of the participants were adherent to the “diet” and experienced a significant decrease in A1C after three months and four years.
Even without a strict ketogenic diet protocol, carbohydrate restriction helped type 1 diabetics. This suggests that carbohydrate restriction is highly effective in improving type 1 diabetes management.
But what about reversing type 1 diabetes? It is highly unlikely that this is possible. According to the current evidence, the most that a diet can do for a patient with type 1 diabetes is halt disease progression and reduce their insulin needs. In cases where the patient is still able to produce some insulin, it is possible for them to be taken off of insulin medication completely with the help of the right diet and healthcare professional.
5.1. Two Important Considerations for The Ketogenic Diet & Type 1 Diabetes
If we look closely at the paleolithic-ketogenic diet that the 19-year-old male implemented, we can find some clues to his outstanding success. The researchers made two important adjustments to the classic ketogenic diet that helped the subject halt disease progression, restore some insulin production, and manage type 1 diabetes without any medication.
1. Vitamin D Supplementation**
Vitamin D helps modulate the innate and adaptive immune responses. This means that it can help prevent and reverse the autoimmune issues that commonly cause type 1 diabetes.
In fact, it is important for everyone to supplement with vitamin d3 or daily sun exposure due to the potential consequences of Vitamin D deficiency.
For example, infants and young children who are vitamin D deficient may be imprinted for the rest of their lives with increased risks of type 1 diabetes, multiple sclerosis, rheumatoid arthritis, and many common cancers.
The simplest way to obtain vitamin D is from moderate exposure to sunlight. For more specific guidelines, many experts suggest supplementing daily with 4,000 IU vitamin D3 without sun exposure or 2,000 IU plus 12–15 minutes of midday sun.
2. The Elimination of Immune System Provoking Foods From The Diet**
Wheat and cow’s milk have been reported to cause strong immune system reactions in type 1 diabetic patients. Something that occurs less often in nondiabetics.
Consumption of cow’s milk has also repeatedly been shown to increase the risk of type 1 diabetes. Some scientists suggest that the milk protein may promote autoimmune processes and give rise to the condition. In fact, two case reports from the literature found that the classic ketogenic diet, which contains a significant amount of dairy, lead to the development of type 1 diabetes in a couple of children with epilepsy.
This doesn’t indicate that dairy can cause type 1 diabetes, but it most definitely can be an accelerator of the disease. Wheat sensitivities may also accelerate the condition by causing gut issues that make type 1 diabetes harder to manage.
The paleolithic-ketogenic diet limits wheat, dairy, and carbohydrate consumption making it the most promising type 1 diabetes diet we know of so far. This is because it not only normalizes glucose levels but may also halt autoimmune processes mediated by milk protein and wheat gluten as well.
5.2. The Takeaway — What is The Best Type 1 Diabetes Diet?
Type 1 diabetes and the keto diet may be the best match for some diabetes patients. In fact, the current data suggest that both low carb and ketogenic diets are highly effective for improving type 1 diabetes management.
Overall, the roadmap for an ideal type 1 diabetes diet may look something like this:
- Follow a ketogenic diet (less than 30 grams of carbohydrates per day)
- Restrict the consumption of dairy and wheat products to see if insulin production improves
- Supplement with vitamin D3
Although these three dietary rules seem simple enough to follow, diabetes patients are likely to experience dramatic changes throughout the body. This will include lower blood sugar levels, decreases in A1C, changes in insulin sensitivity, weight loss, and nutritional ketosis (i.e., healthy increases in ketone level, not diabetic ketoacidosis).
As a result, diabetes medication dosages — insulin dose in particular — will likely need adjustment to accommodate the changes in carb intake and blood glucose levels.
This is why it is vital to work together with your doctor while implementing any major dietary change, such as a ketogenic or low carb diet, to ensure effectiveness and safety.
5.3. Is The Keto Diet Safe For Type 1 Diabetes?
Though the keto diet is safe and effective for weight loss and type 2 diabetes management, those with type 1 diabetes will require closer monitoring and diabetes medication adjustments to ensure safety. If carbohydrate intake and insulin dose are not changed simultaneously on a low carb or keto diet, the risk of hypoglycemia increases significantly.
Once this is addressed, it is important to ensure that the keto or low carb diet is well-formulated with plenty of healthy fats, low-carb vegetables, and enough calories (so that you don’t lose weight unexpectedly).
6. Random Comments
I’m type 1 and doing Keto. You will have to adjust your insulin and even with very low carb meals I still have to do a small bolus. I have improved my a1c dramatically. It will be very frustrating at first but worth it if you stick with it.
Did you run into any problems at first? When I first was diagnosed I had lost
about 20 lbs within a month. How is your weight loss compared to when you were
diagnosed?
Yeah I would have high blood sugars at first because I was always told protein
is the “free food” that doesn’t require any insulin then occasionally low blood
sugars trying to correct the highs. The weight loss is slower than when i was
first diagnosed, but faster than any other diet I’ve tried.
Short answer: Yes, keto diets can be very useful for type 1 diabetes.
Longer answer: You can’t eliminate the need for insulin. On the other hand, your insulin doses will be much more predictable when your carbs are very low, since carbs drive the need for insulin. You’ll likely be able to control your blood sugar much better.
For more info read Dr. Bernstein’s Diet Solution. He is a doctor and a type 1 diabetic and this book is about his experience using keto as a treatment both for himself and his patients.
Yes! You can absolutely do keto and have T1D. I’m T1D and I’ve been doing keto since early February (lazy keto, then stricter keto starting around May). My blood sugars have been more stable, my A1C is down, I have so. much. energy! I’ve also lost close to 20lbs already, so that’s a bonus too. I very rarely go above a 200 bg any more. When I told my endo I started doing keto, she congratulated me and told me to keep it up and to remember to drink enough water. It’s been so so great.
The only “problem” I’ve had is when I go low (not often, but hey lows happen) and had to quickly find food to put in me to get my bg up because I was still dropping. It was also after physical activity (swimming, always my downfall) so I honestly should’ve made sure to eat something beforehand.
Keto is absolutely a great diet for T1D though. I’ve halved the amount of insulin I’m taking daily and most of it just comes from my basal rate. I would recommend it to anyone. You just have to be open to the idea that you might have to break ketosis to bring up a low. That’s about it though.
My understanding is that insulin plays an important role in the prevention of ketoacidosis. If your keto levels get very high, it does become dangerous. Insulin prevents this in a normal person, but with type 1 diabetes you’d have to be extra vigilant. It’s doable but definitely worth talking to a doctor who knows his keto to understand how to manage it.
Take extra care if exercising as exercising on keto spikes ketones, which again is fine for a normal person but is where the problems for a type 1 diabetic are most likely.
This is in regard to T2.
I just wanted to share to encourage anyone who needs it.
I am 46f and was diagnosed with diabetes at the end of October. I have been prediabetic for years and stupidly did nothing about it. Once i got the diagnosis it scared me into action. I had a bit of trouble sticking to it over the holidays and a few celebrations (anniversary, birthdays) but I did my best. I lost 27.6 pounds, but I was disappointed I didn’t lose more.
I went to the doctor yesterday and got bloodwork and my A1C went from 7.9 to 5.7. I’m barely even pre diabetic now!
I was shocked. I was hoping that my A1C would be lower and motivate me to keep going but I never thought I’d see such an improvement so quickly. I’m gonna keep going. I have more weight to lose and don’t ever want to be diabetic again.
So to all of you out there: Stick to it! Even if you don’t think you’re doing well enough, whatever you are doing is making you healthier.
EDIT: For everyone saying I didn’t reverse my diabetes: I do understand that if I go back to my old ways I will quickly be diabetic again. After I got my diagnosis I did not take any meds, just diet and exercise and have lowered my A1C to almost normal levels. Reversed, remission, still diabetic but managing it, I did not fully think through the way those terms are used when I posted. I was happy (and a little tipsy lol) and made a post. I do understand that it is more complicated than I implied.
And even if this was a T1, they can significantly improve their health with keto and use a lot less medication - even a lot less insulin since it is an input function:
f(required insulin) = c x consumed carbs
The less carbs you consume, the less insulin you need (true for both T1 and T2).
Good Videos from an english GP Dr David Unwin on this - his NHS practice has the lowest amount of prescriptions and is a statistical anomaly for NHS. And he gets many patients to remission (the T2s)
Probably T2.
When my blood sugars and A1C were high, I decided to do keto because it made sense to me to lower my glucose levels and it worked - my A1C went from 8.9 (probably artificially high because I was taking Prednisone because of a nasty bout of COVID) to 6.2 in three months through diet alone. My morning blood sugars are still a little higher than I’d like so I was looking up information on how to lower fasting blood sugars from what I assumed would be a reliable source - the American Diabetes Association. After poking around the site a little bit, I was confronted with the “diabetic plate” recommendation which is essentially a low-fat, high-carb method of eating. They even show an example plate of tofu, broccoli and what looks like maybe quinoa or barley? That’s their perfect example of healthy for a diabetic? Assuming it’s barley, if I plug that into my calculator and without sauces (and it suspiciously looks like it has sweet chili sauce) that plate would have 67 carbs, 48 net! That would spike my blood sugar like nothing else. Surely somewhere on the site it talked about keto and low carb?
Eventually, I found it, buried in a not prominent place where it compared many different types of meal plans, in this very ecumenical place, where it actually says, the low-carbohydrate eating pattern improved A1C more, and in trials of varying lengths, lowered triglycerides, raised HDL-C, lowered blood pressure, and resulted in greater reductions in diabetes medication (111). Finally, in another meta-analysis comparing low-carbohydrate to high-carbohydrate eating patterns, the larger the carbohydrate restriction, the greater the reduction in A1C, though A1C was similar at durations of 1 year and longer for both eating patterns." But believe me, you had to wade through a ton to find this and they don’t mention that the similar A1C at the end of the year was after the low carb group was removed from a ton of medications. So this is on their research page, but they still recommend the “diabetic plate” thing?
So I did some research and looked at the archives on r/keto about it, and apparently, this really is a thing, that the ADA has had a history of not recommending low carb for diabetes control. I was pretty shocked. It’s no wonder that it’s hard to find medical professionals that are on board with this way of eating if what should be trusted medical institutions aren’t even doing it.
As a medical professional, I strongly encourage and educate my patients on the importance of a low carb diet. I’ve had heated discussions with other providers who worry more about rising lipid levels than they do about the overall big picture when it comes to diabetes. Diabetes is NOT a sugar problem. It’s a vascular problem. It clogs all the vessels in the body much faster than lipids do ( if they really do-lots of research to suggest they don’t). Time and again the patients that take my advice lower their A1C’s, lose weight, get off meds and in the long run LOWER their lipid panel as well! Always remember any MD,DO, NP or PA is only as good as the research they do. If you ever come across one that doesn’t understand the benefits of a low carb diet- hit the door and find someone that does.
I didn’t verify this, but it seems par for the course. Post was from 2022.
The top four donors to the ADA are all drug companies that make a fortune selling insulin. Together they donate millions. The last thing they want is people coming off insulin by following a low carb diet or they would all go bankrupt. I’m afraid that the ADA has been bought by the lobbies. The CEO actually reversed her diabetes by following a low carb diet, while all the time recommending a low fat diet to the members of the ADA. So there you have it; money speaks.

Unverified, but interesting if true.
Added fun fact, the first diabetic cookbook published a year or two before insulin recommended a forty gram net carb diet. Meal plans with macros for everything, protein and fat heavy…
Sound familiar?
My radical head and neck surgery last September they said I would be in five or six days. My doc ordered keto, 20g net. I manage my T2 entirely with keto and activity and I told them I would just fast. Not eating their food. Hubby was allowed to bring in protein shakes and yogurt.
They thought my mandatory insulin pump was broken after surgery because I never went over 140. Hit my normal 85 or so in less than eighteen hours.
I had significantly less bruising and swelling, needed less pain meds and was out in three days. Great scar healing too.
The only mystery to me was how the hell that hospital could burn beef and chicken broth so badly every day, and why the sugar free jello was liquid.
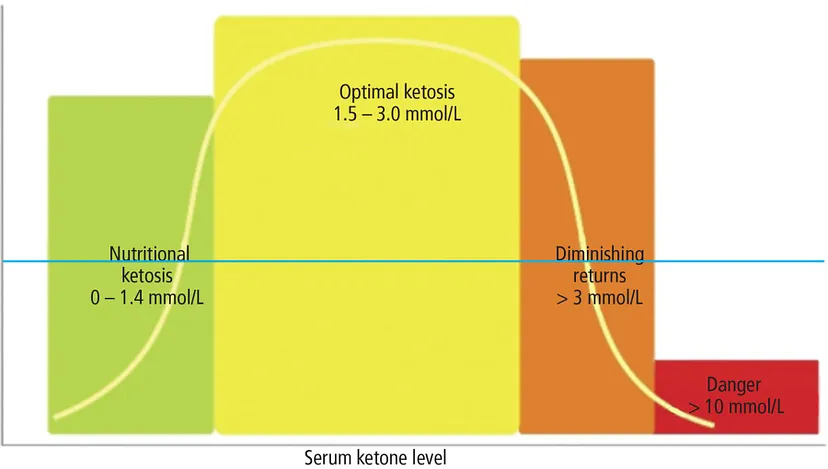
I’m type 1 and been carnivore for a year it’s working well for me but I found you do have to ease yourself into it slowly the main issues as I understand it is when you go into ketosis you have to keep an eye on your ketones just to make sure you not heading towards ketoacidosis I aim for between 2 and 3 on the ketones but if it starts flying up toward 5 or 6 I reintroduce some carbs for a couple of days just to bring it back down and under control The first two months was a rough ride with stomach complaints headaches and some higher blood pressures but it all came good after that
-
Is The KETO DIET Right For A Type 1 Diabetic? - YouTube
-
Seems balanced. I would argue against the cholesterol portion, high LDL should only be bad if you have a sulfate deficiency.
I have eaten the keto way for 10 years. My A1c has consistently been 5.6 since. I was diagnosed type 1 in 1984 (37 years ago). For my body, this is the best my blood sugars have ever been. I recommend reading Dr. Richard Bernstein’s book Diabetes Solution.